Providers must verify TRICARE eligibility for beneficiaries at the time of service. Providers should ensure the patient has a valid Common Access Card (CAC), uniformed services ID card or eligibility authorization letter. Be sure to check the expiration date and make a copy of both sides of the ID card for your patient files.
Verify in self-service.
TRICARE is the secondary payer to all health benefits and insurance plans, with the exception of Medicaid, Indian Health Services and other public programs identified by the government. Always check for OHI and status of OHI with the patient at each visit.
TRICARE beneficiaries can include active duty military and families, retired military and families and survivors, as well as Reserve/Guard and their families.
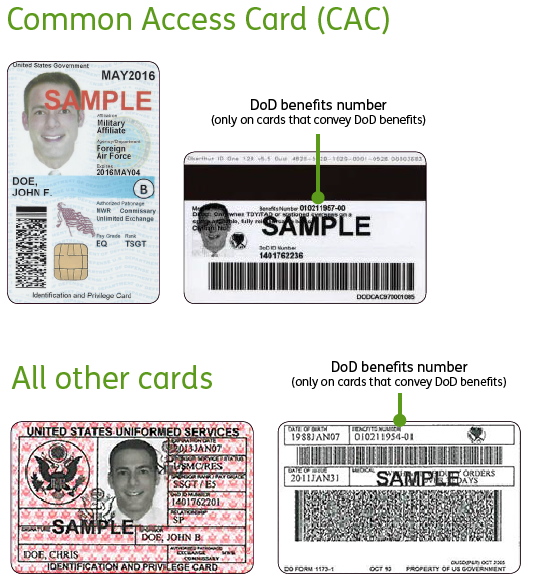
A CAC or ID card alone does not prove TRICARE eligibility. Providers should verify eligibility with Humana Military. The quickest, easiest way to do this is through provider self-service. Active Duty Service Members (ADSM), family members over age 14, retirees and family members will have one of two valid military ID cards shown below.
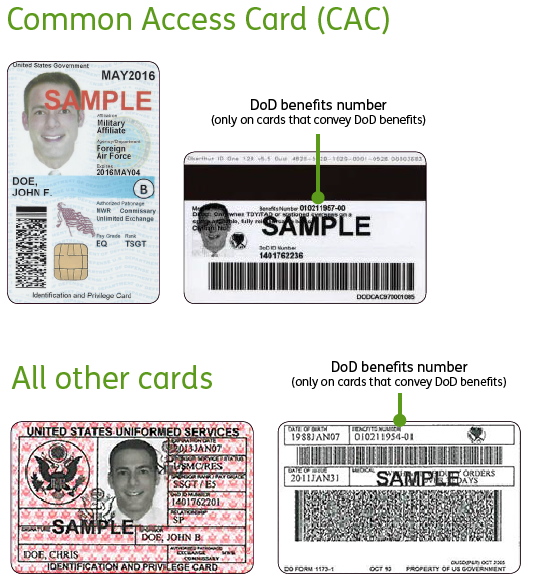
Possible ID numbers you may encounter include:
SSN: a nine-digit number no longer on ID cards, which is acceptable for claims submissions (The sponsor’s SSN is acceptable on family member claims). DoD ID number: a 10-digit number on the front of ID cards, which is not acceptable for claims submissions.
DBN: an 11-digit number on the back of some ID cards, which is acceptable for claims submissions (do not include any dashes).
Be sure to check:
Humana Military’s web-based eligibility check option allows you to use either the sponsor SSN or the DBN member ID to verify eligibility. A current approved referral/authorization number for the patient also works when using our web-based eligibility check.
All eligible family members and survivors age 75 or older are issued permanent ID cards. These cards should read INDEF (i.e., indefinite) in the expiration date box.
ADFMs remain eligible for TRICARE Prime and TRICARE Select while the sponsor is on active duty. However, once the sponsor retires from active duty, the sponsor and his or her family members who are entitled to premium-free Medicare Part A must also have Medicare Part B to keep their TRICARE benefits.
TRICARE Reserve Select (TRS), TRICARE Retired Reserve (TRR), CHCBP and US Family Health Plan (USFHP) beneficiaries are not required to have Medicare Part B to remain covered under these programs.
A TRICARE For Life (TFL) beneficiary with an ID card that reads NO in the Civilian box may still use TFL if he or she has both Medicare Part A and Medicare Part B.
Beneficiaries who are dual-eligible will have Medicare Part A and Part B and TRICARE.
National Guard and Reserve Component members are entitled to medical care coverage under TRICARE while in performance of military duties or if they have incurred or aggravated a medical condition resulting from military service. If information in your records indicates this may be the case, please file your claim with Humana Military for review and adjudication.